Rheumatoid arthritis (RA) is a chronic autoimmune condition that causes inflammation, pain, and stiffness in the joints. Unlike osteoarthritis, which results from wear and tear, RA occurs when the immune system mistakenly attacks the synovium (the lining of the joints). This leads to inflammation, swelling, and, over time, joint damage and disability.
While there is no cure for RA, several rheumatoid arthritis treatments can help manage symptoms, slow disease progression, and improve quality of life.
This article provides a detailed exploration of the various RA treatment options, including medications, therapies, lifestyle changes, and alternative treatments. By understanding these options, patients and caregivers can make informed decisions about managing rheumatoid arthritis effectively.
Why Early Treatment Matters
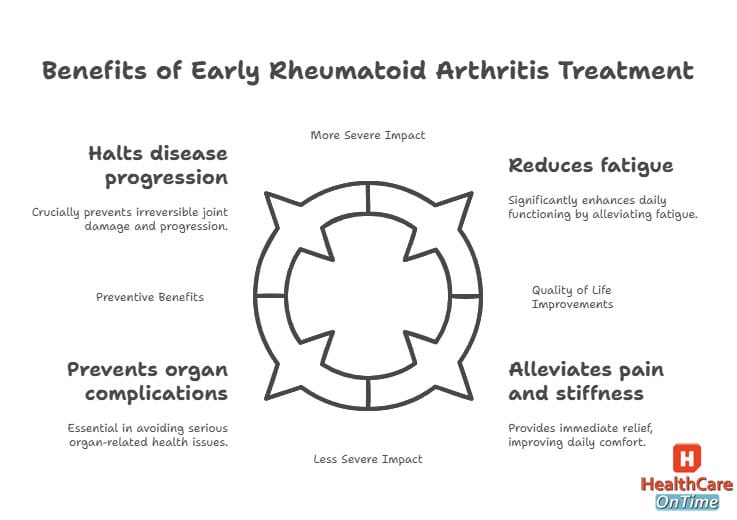
Rheumatoid arthritis is a progressive disease, meaning it worsens over time if left untreated. Early intervention is crucial because it can:
- Prevent Joint Damage: Untreated RA can lead to irreversible joint damage and deformities. Early treatment with disease-modifying antirheumatic drugs (DMARDs) can slow or even halt this progression.
- Improve Quality of Life: Effective RA treatment options can reduce pain, stiffness, and fatigue, allowing patients to stay active and independent.
- Reduce Long-Term Complications: RA doesn’t just affect the joints—it can also impact the heart, lungs, and other organs. Early treatment lowers the risk of these complications.
What to Expect in This Guide?
In the following sections, we’ll dive deep into the various rheumatoid arthritis treatments available today. Here’s a sneak peek of what’s covered:
- Medications: From traditional DMARDs to cutting-edge biologics, we’ll explore how these drugs work, their benefits, and potential side effects.
- Therapies: Learn how physical therapy, occupational therapy, and even joint surgery can help manage RA symptoms and improve mobility.
- Lifestyle Changes: Discover how exercise, diet, and stress management can complement medical treatments and enhance your overall well-being.
- Alternative Treatments: Explore options like acupuncture, herbal supplements, and mind-body therapies that may provide additional relief.
- Emerging Treatments: Get the latest updates on groundbreaking therapies like JAK inhibitors and stem cell therapy.
By the end of this guide, you’ll have a clear understanding of the RA treatment options available and how to create a personalized plan that works for you.
Understanding Rheumatoid Arthritis
Rheumatoid arthritis (RA) is not just a disease of the joints—it’s a systemic condition that can affect the entire body. To understand how rheumatoid arthritis treatments work, it’s essential to first understand what RA is, how it develops, and how it impacts those who live with it.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis is an autoimmune disorder, meaning the body’s immune system mistakenly attacks its own tissues. In the case of RA, the immune system targets the synovium—the thin membrane that lines the joints. This leads to inflammation, which causes:
- Swelling: The joints become swollen and tender.
- Pain: Persistent pain, especially during movement.
- Stiffness: Morning stiffness that lasts for hours is a hallmark of RA.
Over time, chronic inflammation can damage the cartilage and bone within the joint, leading to deformities and loss of function. Unlike osteoarthritis, which is caused by wear and tear, RA is a systemic disease that can also affect other organs, including the heart, lungs, and eyes.
Causes and Risk Factors
The exact cause of RA is unknown, but researchers believe it results from a combination of genetic and environmental factors:
Genetic Factors
- Family History: People with a family history of RA are at higher risk.
- Specific Genes: Certain genes, such as HLA-DR4, are associated with an increased risk of developing RA.
Environmental Triggers
- Infections: Viral or bacterial infections may trigger RA in genetically predisposed individuals.
- Smoking: Smoking is a significant risk factor for RA and can worsen the disease.
- Hormonal Changes: Women are more likely to develop RA, suggesting a link to hormonal changes.
Symptoms of Rheumatoid Arthritis
RA symptoms can vary from person to person, but common signs include:
Joint Symptoms
- Pain and Swelling: Affected joints are often tender, warm, and swollen.
- Stiffness: Morning stiffness that lasts more than 30 minutes is a key symptom.
- Symmetrical Involvement: RA typically affects the same joints on both sides of the body (e.g., both hands or both knees).
Systemic Symptoms
- Fatigue: Many people with RA experience extreme tiredness.
- Fever: Low-grade fever may occur during flare-ups.
- Weight Loss: Unintended weight loss is common in active RA.
Extra-Articular Manifestations
RA can also affect other parts of the body, leading to complications such as:
- Rheumatoid Nodules: Firm lumps under the skin, often near joints.
- Lung Disease: Inflammation of the lung tissue (interstitial lung disease).
- Cardiovascular Issues: Increased risk of heart disease and stroke.
Diagnosing Rheumatoid Arthritis
Early diagnosis is critical for effective rheumatoid arthritis treatments. The diagnostic process typically involves:
Medical History and Physical Exam
- A doctor will ask about symptoms, family history, and risk factors.
- They will also examine the joints for swelling, tenderness, and range of motion.
Blood Tests
- Rheumatoid Factor (RF): An antibody present in about 80% of RA patients.
- Anti-Cyclic Citrullinated Peptide (anti-CCP): A more specific marker for RA.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These tests measure inflammation levels.
Imaging Tests
- X-rays: To detect joint damage and monitor disease progression.
- MRI and Ultrasound: These can reveal early signs of inflammation and joint damage.
The Emotional and Social Impact of RA
Living with rheumatoid arthritis is not just a physical challenge—it’s an emotional and social one as well. Many patients experience:
- Depression and Anxiety: Chronic pain and disability can take a toll on mental health.
- Social Isolation: Difficulty participating in activities can lead to feelings of loneliness.
- Financial Strain: The cost of RA medications and treatments can be overwhelming.
Understanding these challenges is essential for providing holistic rheumatoid arthritis treatments that address not just the physical symptoms but also the emotional and social well-being of patients.
Medications for Rheumatoid Arthritis
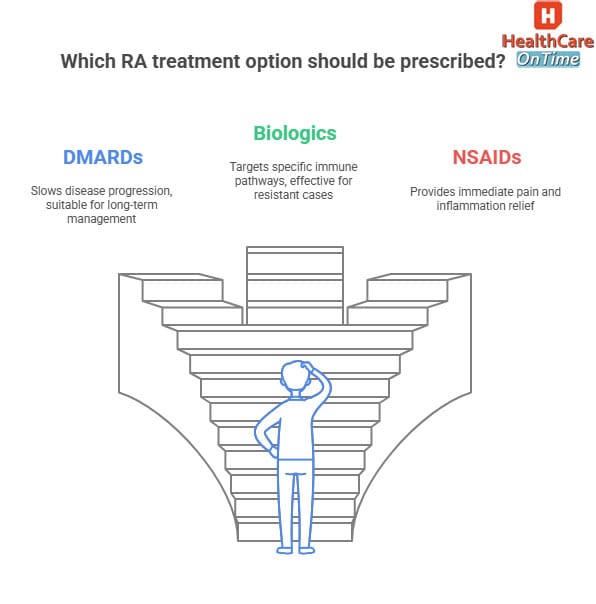
Medications are the cornerstone of rheumatoid arthritis treatments. They aim to reduce inflammation, relieve pain, and slow disease progression. The right combination of RA medications can help patients manage their symptoms effectively and maintain their quality of life.
In this section, we’ll explore the main categories of medications used to treat RA, including disease-modifying antirheumatic drugs (DMARDs), biologic DMARDs, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids.
Disease-Modifying Antirheumatic Drugs (DMARDs)
What Are DMARDs?
DMARDs are the first line of treatment for rheumatoid arthritis. Unlike medications that only relieve symptoms, DMARDs target the underlying cause of RA by suppressing the overactive immune system and reducing inflammation.
How Do DMARDs Work?
- Immune Suppression: DMARDs slow down the immune system’s attack on the joints.
- Inflammation Reduction: They reduce the production of inflammatory chemicals like cytokines.
- Joint Protection: By controlling inflammation, DMARDs prevent joint damage and deformities.
Common DMARDs
- Methotrexate: The most commonly prescribed DMARD, often considered the gold standard for RA treatment.
- Hydroxychloroquine: Used for mild RA or in combination with other DMARDs.
- Sulfasalazine: Effective for both RA and inflammatory bowel disease.
- Leflunomide: An alternative to methotrexate for patients who cannot tolerate it.
Benefits of DMARDs
- Slow Disease Progression: DMARDs can significantly reduce joint damage over time.
- Improve Symptoms: Many patients experience reduced pain, swelling, and stiffness.
- Long-Term Use: DMARDs are safe for long-term use when monitored properly.
Side Effects of DMARDs
- Liver Damage: Regular blood tests are needed to monitor liver function.
- Bone Marrow Suppression: DMARDs can lower white blood cell counts, increasing infection risk.
- Gastrointestinal Issues: Nausea, vomiting, and diarrhea are common side effects.
Biologic DMARDs
What Are Biologic DMARDs?
Biologic DMARDs are a newer class of medications that target specific components of the immune system, such as cytokines (proteins that promote inflammation). They are often used when traditional DMARDs are not effective.
How Do Biologic DMARDs Work?
- Targeted Therapy: Biologics block specific molecules involved in the inflammatory process, such as TNF-alpha, IL-6, or B-cells.
- Precision: Because they target specific pathways, biologics are highly effective with fewer systemic side effects.
Common Biologic DMARDs
- TNF Inhibitors: Etanercept (Enbrel), adalimumab (Humira), and infliximab (Remicade).
- IL-6 Inhibitors: Tocilizumab (Actemra).
- B-Cell Inhibitors: Rituximab (Rituxan).
- JAK Inhibitors: Tofacitinib (Xeljanz) and baricitinib (Olumiant).
Benefits of Biologic DMARDs
- Rapid Relief: Many patients experience significant improvement within weeks.
- Joint Protection: Biologics can prevent joint damage and deformities.
- Improved Quality of Life: Reduced pain and stiffness allow patients to resume daily activities.
Side Effects of Biologic DMARDs
- Increased Infection Risk: Biologics suppress the immune system, making patients more susceptible to infections.
- Allergic Reactions: Some patients may experience injection site reactions or more severe allergic responses.
- High Cost: Biologics are expensive, and access may be limited for some patients.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
What Are NSAIDs?
NSAIDs are medications that reduce pain and inflammation but do not slow disease progression. They are often used for symptom relief in combination with DMARDs or biologics.
How Do NSAIDs Work?
- Inhibition of COX Enzymes: NSAIDs block the production of prostaglandins, chemicals that cause pain and inflammation.
- Symptom Relief: They provide quick relief from pain, swelling, and stiffness.
Common NSAIDs
- Ibuprofen (Advil, Motrin): Available over-the-counter and by prescription.
- Naproxen (Aleve): Longer-lasting than ibuprofen.
- Celecoxib (Celebrex): A COX-2 inhibitor with fewer gastrointestinal side effects.
Benefits of NSAIDs
- Quick Relief: NSAIDs provide fast relief from pain and inflammation.
- Accessibility: Many NSAIDs are available over-the-counter.
- Versatility: They can be used for both RA and other types of pain.
Side Effects of NSAIDs
- Gastrointestinal Issues: Stomach ulcers and bleeding are common with long-term use.
- Kidney Damage: NSAIDs can impair kidney function, especially in older adults.
- Cardiovascular Risks: Long-term use may increase the risk of heart attack or stroke.
Corticosteroids
What Are Corticosteroids?
Corticosteroids are potent anti-inflammatory drugs that provide rapid relief from RA symptoms. They are often used for short-term flare-ups or as a bridge therapy while waiting for DMARDs to take effect.
How Do Corticosteroids Work?
- Immune Suppression: Corticosteroids suppress the immune system and reduce inflammation.
- Rapid Relief: They provide quick relief from pain, swelling, and stiffness.
Common Corticosteroids
- Prednisone: The most commonly prescribed oral corticosteroid.
- Methylprednisolone: Often used for severe flare-ups.
- Intra-Articular Injections: Corticosteroids can be injected directly into affected joints for localized relief.
Benefits of Corticosteroids
- Fast-Acting: Corticosteroids provide rapid relief during flare-ups.
- Versatility: They can be taken orally, injected, or applied topically.
- Bridge Therapy: They are useful while waiting for DMARDs or biologics to take effect.
Side Effects of Corticosteroids
- Weight Gain: Fluid retention and increased appetite are common.
- Osteoporosis: Long-term use can weaken bones.
- Increased Infection Risk: Corticosteroids suppress the immune system.
- Mood Changes: Some patients experience mood swings or depression.
Therapies for Rheumatoid Arthritis
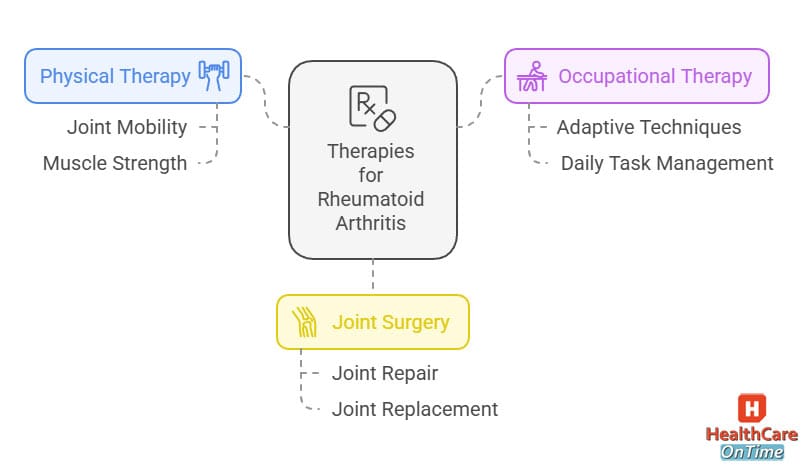
While medications are the foundation of rheumatoid arthritis treatments, therapies play a crucial role in managing symptoms, improving joint function, and enhancing quality of life. These therapies are often used in combination with RA medications to provide a holistic approach to treatment.
In this section, we’ll explore the key therapies available for RA patients, including physical therapy, occupational therapy, and joint surgery.
Physical Therapy for RA
What Is Physical Therapy?
Physical therapy involves exercises and techniques designed to improve joint mobility, strengthen muscles, and reduce pain. A physical therapist tailors the program to the patient’s specific needs, ensuring safe and effective treatment.
How Does Physical Therapy Help?
- Improves Joint Mobility: Range-of-motion exercises help maintain flexibility in affected joints.
- Strengthens Muscles: Strengthening exercises support weakened joints and reduce strain.
- Reduces Pain: Techniques like manual therapy and ultrasound can alleviate pain and inflammation.
- Enhances Overall Fitness: Low-impact aerobic exercises improve cardiovascular health and endurance.
Common Physical Therapy Techniques
- Range-of-Motion Exercises: Gentle movements to maintain or improve joint flexibility.
- Strengthening Exercises: Resistance training to build muscle around affected joints.
- Low-Impact Aerobics: Activities like swimming, cycling, or walking to improve fitness without stressing the joints.
- Manual Therapy: Hands-on techniques to mobilize joints and soft tissues.
Benefits of Physical Therapy
- Pain Relief: Regular therapy can significantly reduce pain and stiffness.
- Improved Mobility: Patients often experience better joint function and flexibility.
- Prevention of Deformities: Strengthening and stretching exercises can prevent joint deformities.
Occupational Therapy for Rheumatoid Arthritis
What Is Occupational Therapy?
Occupational therapy focuses on helping patients perform daily activities with less pain and strain. An occupational therapist provides tools, techniques, and modifications to make tasks easier and more manageable.
How Does Occupational Therapy Help?
- Adaptive Techniques: Teaches patients how to perform tasks in ways that reduce joint stress.
- Assistive Devices: Recommends tools like jar openers, button hooks, or ergonomic utensils.
- Energy Conservation: Strategies to manage fatigue and prioritize activities.
- Home and Workplace Modifications: Adjustments to create a more RA-friendly environment.
Common Occupational Therapy Techniques
- Joint Protection Strategies: Techniques to minimize strain on affected joints.
- Splints and Braces: Custom devices to support and stabilize joints.
- Task Simplification: Breaking down tasks into smaller, manageable steps.
- Education: Teaching patients about RA and how to manage it effectively.
Benefits of Occupational Therapy
- Improved Independence: Patients can perform daily tasks with less assistance.
- Reduced Pain: Proper techniques and tools minimize joint strain.
- Enhanced Quality of Life: Patients feel more confident and capable in their daily lives.
Joint Surgery for RA
What Is Joint Surgery?
In severe cases of RA, joint surgery may be necessary to repair or replace damaged joints. Surgery is typically considered when medications and therapies no longer provide adequate relief.
Types of Joint Surgery
- Synovectomy: Removal of the inflamed synovium to reduce pain and swelling.
- Joint Fusion: Fusing bones together to stabilize a joint and reduce pain.
- Joint Replacement: Replacing a damaged joint with an artificial one (e.g., knee or hip replacement).
How Does Joint Surgery Help?
- Pain Relief: Surgery can significantly reduce or eliminate pain in severely affected joints.
- Restored Function: Patients often regain mobility and independence.
- Improved Quality of Life: Surgery can allow patients to resume activities they once enjoyed.
Benefits of Joint Surgery
- Long-Term Relief: Many patients experience lasting pain relief and improved function.
- Enhanced Mobility: Joint replacement surgery can restore near-normal movement.
- Prevention of Further Damage: Surgery can prevent additional joint damage and deformities.
Lifestyle Changes for Rheumatoid Arthritis
While rheumatoid arthritis treatments like medications and therapies are essential, lifestyle changes can play a significant role in managing symptoms and improving quality of life. These changes are not a substitute for medical treatment but can enhance its effectiveness and help patients feel more in control of their condition. In this section, we’ll explore key lifestyle modifications, including exercise, diet, stress management, and rest.
Exercise
Why Exercise Matters
Regular exercise is one of the most effective ways to manage RA symptoms. It helps maintain joint flexibility, strengthen muscles, and reduce fatigue. Exercise also improves cardiovascular health, mental well-being, and overall quality of life.
Types of Exercise for RA
- Low-Impact Aerobics: Activities like swimming, cycling, and walking are gentle on the joints while improving cardiovascular fitness.
- Strength Training: Light resistance exercises help build muscle around affected joints, providing better support and reducing strain.
- Stretching: Gentle stretching exercises improve flexibility and reduce stiffness.
- Yoga and Tai Chi: These practices combine movement, stretching, and mindfulness, making them ideal for RA patients.
Benefits of Exercise
- Reduced Pain and Stiffness: Regular movement helps keep joints flexible and reduces inflammation.
- Improved Mobility: Exercise enhances joint function and range of motion.
- Better Mental Health: Physical activity releases endorphins, which improve mood and reduce stress.
Tips for Getting Started
- Start Slow: Begin with low-intensity exercises and gradually increase intensity.
- Listen to Your Body: Avoid overexertion and stop if you experience pain.
- Work with a Professional: A physical therapist can design a personalized exercise plan.
Diet
The Role of Diet in RA
A balanced diet rich in anti-inflammatory foods can help reduce RA symptoms and support overall health. While no specific diet can cure RA, certain foods can help manage inflammation and improve well-being.
Anti-Inflammatory Foods
- Fatty Fish: Salmon, mackerel, and sardines are rich in omega-3 fatty acids, which have anti-inflammatory properties.
- Fruits and Vegetables: Berries, leafy greens, and colorful vegetables are packed with antioxidants that fight inflammation.
- Whole Grains: Brown rice, quinoa, and oats provide fiber and nutrients without spiking blood sugar.
- Nuts and Seeds: Almonds, walnuts, and flaxseeds are excellent sources of healthy fats and antioxidants.
Foods to Avoid
- Processed Foods: These often contain trans fats, sugar, and additives that promote inflammation.
- Sugary Snacks: High sugar intake can worsen inflammation and contribute to weight gain.
- Excessive Red Meat: Red meat contains saturated fats that may increase inflammation.
Benefits of a Healthy Diet
- Reduced Inflammation: Anti-inflammatory foods can help lower systemic inflammation.
- Improved Energy Levels: A balanced diet provides the nutrients needed for energy and vitality.
- Better Weight Management: Maintaining a healthy weight reduces strain on joints.
Stress Management
The Link Between Stress and RA
Stress can trigger RA flare-ups and worsen symptoms. Managing stress is crucial for maintaining physical and emotional well-being.
Stress-Relief Techniques
- Meditation: Mindfulness meditation helps calm the mind and reduce stress.
- Deep Breathing: Simple breathing exercises can lower stress levels and promote relaxation.
- Hobbies: Engaging in activities you enjoy, such as painting, gardening, or reading, can distract from pain and reduce stress.
- Social Support: Connecting with friends, family, or support groups can provide emotional comfort.
Benefits of Stress Management
- Fewer Flare-Ups: Lower stress levels can reduce the frequency and severity of RA flare-ups.
- Improved Mental Health: Stress management techniques can alleviate anxiety and depression.
- Better Sleep: Reduced stress often leads to improved sleep quality.
Rest and Sleep
The Importance of Rest
Adequate rest and sleep are essential for managing RA symptoms. Rest allows the body to recover and reduces inflammation, while poor sleep can worsen pain and fatigue.
Tips for Better Sleep
- Stick to a Schedule: Go to bed and wake up at the same time every day.
- Create a Relaxing Environment: Keep your bedroom cool, dark, and quiet.
- Limit Screen Time: Avoid electronic devices before bedtime to improve sleep quality.
- Practice Relaxation Techniques: Deep breathing or gentle stretching before bed can promote relaxation.
Benefits of Rest and Sleep
- Reduced Pain: Proper rest helps the body recover and reduces inflammation.
- Improved Energy Levels: Quality sleep boosts energy and reduces fatigue.
- Better Mood: Adequate rest improves mental clarity and emotional well-being.
Pain Management in RA
Pain is one of the most debilitating symptoms of rheumatoid arthritis, affecting every aspect of a patient’s life. Effective pain management in RA is essential for improving quality of life and maintaining daily function. While medications like NSAIDs and corticosteroids play a key role, there are also non-medical strategies that can help. In this section, we’ll explore a comprehensive approach to managing RA pain, including medications, therapies, and lifestyle adjustments.
Medications for Pain Relief
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- What They Do: NSAIDs reduce pain and inflammation by blocking the production of prostaglandins, chemicals that cause pain and swelling.
- Examples: Ibuprofen (Advil), naproxen (Aleve), and celecoxib (Celebrex).
- Benefits: Provide quick relief from pain and stiffness.
- Side Effects: Long-term use can lead to stomach ulcers, kidney problems, and cardiovascular risks.
Corticosteroids
- What They Do: Corticosteroids are potent anti-inflammatory drugs that provide rapid relief from pain and swelling.
- Examples: Prednisone and methylprednisolone.
- Benefits: Effective for short-term flare-ups and severe pain.
- Side Effects: Long-term use can cause weight gain, osteoporosis, and increased infection risk.
Analgesics
- What They Do: Analgesics, such as acetaminophen (Tylenol), relieve pain but do not reduce inflammation.
- Benefits: Useful for mild to moderate pain without the side effects of NSAIDs.
- Limitations: Not effective for inflammation-related pain.
Heat and Cold Therapy
Heat Therapy
- What It Does: Heat relaxes muscles, improves blood flow, and reduces stiffness.
- When to Use: Ideal for chronic pain or morning stiffness.
- Methods: Heating pads, warm baths, or heated blankets.
- Benefits: Provides immediate relief and improves joint flexibility.
Cold Therapy
- What It Does: Cold reduces swelling and numbs pain by constricting blood vessels.
- When to Use: Best for acute pain or flare-ups.
- Methods: Ice packs, cold compresses, or frozen gel packs.
- Benefits: Reduces inflammation and provides quick pain relief.
Assistive Devices
What Are Assistive Devices?
Assistive devices are tools designed to reduce strain on joints and make daily tasks easier. They are particularly helpful for patients with severe joint damage or limited mobility.
Types of Assistive Devices
- Braces and Splints: Provide support and stability to affected joints.
- Canes and Walkers: Help with balance and reduce pressure on weight-bearing joints.
- Ergonomic Tools: Jar openers, button hooks, and adaptive utensils make daily tasks less painful.
Benefits of Assistive Devices
- Reduced Pain: Devices minimize strain on joints, reducing pain during activities.
- Improved Independence: Patients can perform tasks without assistance.
- Prevention of Further Damage: Reducing joint strain helps prevent additional damage.
Mind-Body Techniques
What Are Mind-Body Techniques?
Mind-body techniques focus on the connection between the mind and body to reduce pain and improve well-being. These methods are particularly helpful for managing chronic pain.
Common Techniques
- Meditation: Mindfulness meditation helps patients focus on the present moment and reduce stress.
- Deep Breathing: Simple breathing exercises can lower stress levels and promote relaxation.
- Yoga and Tai Chi: These practices combine movement, stretching, and mindfulness, making them ideal for RA patients.
Benefits of Mind-Body Techniques
- Reduced Pain Perception: These techniques can change how the brain processes pain signals.
- Improved Mental Health: They reduce stress, anxiety, and depression.
- Enhanced Relaxation: Patients often feel calmer and more in control of their symptoms.
Alternative Therapies
Acupuncture
- What It Does: Acupuncture involves inserting thin needles into specific points on the body to relieve pain and inflammation.
- Benefits: Some patients experience significant pain relief and improved joint function.
- Limitations: Results vary, and more research is needed to confirm its effectiveness for RA.
Massage Therapy
- What It Does: Massage reduces muscle tension, improves circulation, and promotes relaxation.
- Benefits: Helps alleviate pain and stiffness, especially in surrounding muscles.
- Limitations: May not be suitable during active flare-ups.
Herbal Supplements
- What They Do: Supplements like turmeric, ginger, and fish oil have anti-inflammatory properties.
- Benefits: May provide additional pain relief when used alongside conventional treatments.
- Limitations: Always consult a doctor before trying supplements, as they can interact with medications.
Alternative Treatments for Rheumatoid Arthritis
While conventional RA medications and therapies are the foundation of treatment, many patients explore alternative treatments to complement their care. These therapies, often referred to as complementary or integrative medicine, can provide additional relief from symptoms and improve quality of life. However, it’s important to approach these treatments with caution and always consult a healthcare provider before trying them.
In this section, we’ll explore some of the most popular alternative treatments for rheumatoid arthritis, including acupuncture, herbal supplements, massage therapy, and mind-body practices.
Acupuncture
What Is Acupuncture?
Acupuncture is a traditional Chinese medicine technique that involves inserting thin needles into specific points on the body to balance energy flow (known as Qi) and promote healing.
How Does It Help RA?
- Pain Relief: Acupuncture may stimulate the release of endorphins, the body’s natural painkillers.
- Reduced Inflammation: Some studies suggest acupuncture can lower levels of inflammatory markers.
- Improved Joint Function: Patients often report better mobility and reduced stiffness after sessions.
What to Expect
- A licensed acupuncturist will insert needles into specific points, often near affected joints.
- Sessions typically last 30-60 minutes and may require multiple visits for noticeable results.
Benefits
- Non-invasive and generally safe when performed by a trained professional.
- Can provide relief for some patients, especially when combined with conventional treatments.
Limitations
- Results vary, and more research is needed to confirm its effectiveness for RA.
- Not a substitute for RA medications or other proven treatments.
Herbal Supplements
What Are Herbal Supplements?
Herbal supplements are plant-based products that may have anti-inflammatory or pain-relieving properties. Some RA patients use them to complement their treatment plan.
Common Supplements for RA
- Turmeric: Contains curcumin, a compound with potent anti-inflammatory effects.
- Ginger: Known for its anti-inflammatory and antioxidant properties.
- Fish Oil: Rich in omega-3 fatty acids, which can reduce inflammation.
- Green Tea: Contains polyphenols that may help modulate the immune system.
Benefits
- May provide additional relief from pain and inflammation.
- Natural and widely available.
Limitations
- Supplements are not regulated as strictly as medications, so quality can vary.
- Can interact with RA medications, so always consult a doctor before use.
Massage Therapy
What Is Massage Therapy?
Massage therapy involves manipulating the body’s soft tissues to reduce muscle tension, improve circulation, and promote relaxation.
How Does It Help RA?
- Pain Relief: Massage can alleviate muscle tension around affected joints.
- Improved Mobility: Gentle stretching during massage can enhance joint flexibility.
- Stress Reduction: Massage promotes relaxation, which can help manage stress-related flare-ups.
Types of Massage for RA
- Swedish Massage: Gentle and relaxing, ideal for RA patients.
- Deep Tissue Massage: Targets deeper muscle layers but should be used cautiously to avoid joint strain.
- Myofascial Release: Focuses on releasing tension in the connective tissue.
Benefits
- Non-invasive and generally safe.
- Can provide immediate relief from pain and stiffness.
Limitations
- May not be suitable during active flare-ups or for severely inflamed joints.
- Should be performed by a therapist experienced in working with RA patients.
Mind-Body Practices
What Are Mind-Body Practices?
Mind-body practices focus on the connection between mental and physical health to promote healing and well-being. These techniques are particularly helpful for managing chronic pain and stress.
Common Practices
- Yoga: Combines physical postures, breathing exercises, and meditation to improve flexibility and reduce stress.
- Tai Chi: A gentle form of martial arts that involves slow, flowing movements and deep breathing.
- Meditation: Mindfulness meditation helps patients focus on the present moment and reduce stress.
- Biofeedback: Teaches patients to control physiological functions, such as heart rate, to manage pain.
Benefits
- Reduces stress, which can trigger RA flare-ups.
- Improves joint flexibility and overall fitness.
- Enhances mental well-being and emotional resilience.
Limitations
- Requires consistent practice to see results.
- May need to be modified for patients with severe joint damage.
Other Alternative Therapies
Chiropractic Care
- What It Is: A form of manual therapy that focuses on aligning the spine and joints.
- Benefits: May provide relief for some patients, particularly those with spinal involvement.
- Limitations: Not suitable for severely inflamed joints and should be approached with caution.
Hydrotherapy
- What It Is: Exercise or therapy performed in warm water to reduce joint strain.
- Benefits: Improves mobility and reduces pain without stressing the joints.
- Limitations: Requires access to a pool or hydrotherapy facility.
Aromatherapy
- What It Is: The use of essential oils to promote relaxation and reduce stress.
- Benefits: Can enhance mood and reduce stress-related symptoms.
- Limitations: Not a direct treatment for RA but can complement other therapies.
Emerging Treatments and Research
The field of rheumatoid arthritis treatment is constantly evolving, with researchers exploring new ways to manage symptoms, slow disease progression, and even reverse joint damage. While conventional RA medications and therapies remain the standard of care, emerging treatments offer hope for more effective and personalized approaches.
In this section, we’ll explore some of the most promising advancements in rheumatoid arthritis treatments, including JAK inhibitors, stem cell therapy, and gene therapy.
JAK Inhibitors
What Are JAK Inhibitors?
JAK (Janus kinase) inhibitors are a newer class of RA medications that target specific enzymes involved in the immune response. These enzymes, known as JAKs, play a key role in the production of inflammatory cytokines.
How Do JAK Inhibitors Work?
- Targeted Action: JAK inhibitors block the JAK-STAT signaling pathway, which is responsible for producing inflammatory cytokines.
- Oral Administration: Unlike biologics, which are injected, JAK inhibitors are taken orally, making them more convenient for some patients.
Common JAK Inhibitors
- Tofacitinib (Xeljanz): The first JAK inhibitor approved for RA.
- Baricitinib (Olumiant): Another widely used JAK inhibitor.
- Upadacitinib (Rinvoq): A newer option with promising results.
Benefits
- Effective for Moderate to Severe RA: JAK inhibitors can significantly reduce symptoms and slow disease progression.
- Convenience: Oral administration is easier for patients who dislike injections.
- Rapid Relief: Many patients experience improvement within weeks.
Side Effects
- Increased Infection Risk: Like biologics, JAK inhibitors suppress the immune system.
- Blood Clots: Some studies suggest a higher risk of blood clots with certain JAK inhibitors.
- Cost: These medications can be expensive, and insurance coverage may vary.
Stem Cell Therapy
What Is Stem Cell Therapy?
Stem cell therapy is an experimental treatment that uses stem cells to repair damaged tissues and modulate the immune system. While still in the early stages of research, it holds promise for treating autoimmune diseases like RA.
How Does It Help RA?
- Tissue Repair: Stem cells can differentiate into various cell types, potentially repairing damaged cartilage and bone.
- Immune Modulation: Stem cells may help regulate the immune system, reducing inflammation and preventing further joint damage.
Types of Stem Cell Therapy
- Autologous Stem Cells: Derived from the patient’s own body, often from bone marrow or fat tissue.
- Allogeneic Stem Cells: Derived from a donor, offering a more standardized treatment option.
Benefits
- Potential for Long-Term Relief: Stem cell therapy could provide lasting benefits by addressing the root cause of RA.
- Minimally Invasive: Many procedures involve simple injections rather than surgery.
Limitations
- Experimental: Stem cell therapy is not yet widely available or approved for RA.
- Cost: The treatment can be expensive and is often not covered by insurance.
- Risks: Potential side effects include infection and immune rejection.
Gene Therapy
What Is Gene Therapy?
Gene therapy involves modifying a patient’s genes to treat or prevent disease. In the context of RA, researchers are exploring ways to reprogram immune cells to stop attacking the joints.
How Does It Help RA?
- Immune Reprogramming: Gene therapy could “teach” immune cells to tolerate joint tissues instead of attacking them.
- Targeted Treatment: By addressing the root cause of RA, gene therapy has the potential to provide long-term remission.
Current Research
- CAR-T Cell Therapy: Originally developed for cancer, this approach is being adapted for autoimmune diseases like RA.
- CRISPR Technology: A gene-editing tool that could correct genetic mutations linked to RA.
Benefits
- Potential for a Cure: Gene therapy could offer a one-time treatment that addresses the underlying cause of RA.
- Personalized Medicine: Treatments could be tailored to each patient’s genetic profile.
Limitations
- Experimental: Gene therapy is still in the early stages of research and not yet available for RA.
- Ethical Concerns: The long-term effects of gene editing are not fully understood.
- Cost: If approved, gene therapy is likely to be expensive.
Other Emerging Treatments
Microbiome Therapy
- What It Is: Research suggests that gut bacteria play a role in autoimmune diseases. Microbiome therapy involves using probiotics, prebiotics, or fecal transplants to restore a healthy balance of gut bacteria.
- Potential Benefits: Could reduce inflammation and improve immune function.
Nanotechnology
- What It Is: Nanoparticles are being developed to deliver drugs directly to inflamed joints, minimizing side effects.
- Potential Benefits: More targeted and effective treatment with fewer systemic effects.
Biologic Innovations
- What It Is: Researchers are developing next-generation biologics with improved targeting and fewer side effects.
- Potential Benefits: Enhanced efficacy and convenience for patients.
Taking Control of Your Rheumatoid Arthritis Journey
Rheumatoid arthritis (RA) is a complex and challenging condition, but it doesn’t have to define your life. With the right rheumatoid arthritis treatments, you can manage your symptoms, slow disease progression, and maintain your quality of life. From RA medications like DMARDs and biologics to therapies, lifestyle changes, and emerging treatments, there are more options than ever to help you live well with RA.
Key Takeaways
- Early Diagnosis and Treatment Are Crucial: The sooner you start treatment, the better your chances of preventing joint damage and achieving remission.
- Medications Are the Foundation: Disease-modifying antirheumatic drugs (DMARDs), biologic DMARDs, and JAK inhibitors are highly effective in controlling inflammation and slowing disease progression.
- Therapies Complement Medications: Physical therapy, occupational therapy, and joint surgery can improve mobility, reduce pain, and enhance independence.
- Lifestyle Changes Make a Difference: Exercise, a healthy diet, stress management, and adequate rest can significantly improve your symptoms and overall well-being.
- Emerging Treatments Offer Hope: Advances like JAK inhibitors, stem cell therapy, and gene therapy are paving the way for more effective and personalized treatments.
Living with rheumatoid arthritis can be difficult, but it’s important to remember that you are not alone. Millions of people around the world are managing RA successfully, and with the right support and treatment, you can too.
Whether it’s through RA medications, therapies, lifestyle changes, or emerging treatments, there are countless ways to reduce your symptoms and improve your quality of life.
Take it one day at a time, celebrate your progress, and don’t hesitate to lean on your healthcare team, family, and friends for support. Together, we can face the challenges of RA and work toward a brighter, healthier future.
Sources
Ref Links:
- Arthritis Foundation – “Rheumatoid Arthritis Treatment”
- Mayo Clinic – “Rheumatoid Arthritis: Diagnosis and Treatment”
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) – “Rheumatoid Arthritis”
- WebMD – “Rheumatoid Arthritis Treatments”
- Healthline – “Rheumatoid Arthritis Treatment Options”
- American College of Rheumatology – “Rheumatoid Arthritis”
- Cleveland Clinic – “Rheumatoid Arthritis: Management and Treatment”
- PubMed Central – “Advances in the Treatment of Rheumatoid Arthritis”
- Harvard Health Publishing – “Rheumatoid Arthritis: What You Need to Know”
- National Health Service (NHS) – “Rheumatoid Arthritis: Treatment”