Often considered as the planet's oldest known disease, presence of
Osteoarthritis has been documented in the skeletons of dinosaurs roughly around
5 to 7 crore years ago. It was frequently observed in numerous Egyptian
mummies and in ancient skeletons from England. Unlike today, Osteoarthritis of the
shoulders and spine were more OSTEOARTHRITIS common than the knee
joints illustrating more of physical labor and less obesity a in the foregone time.
Osteoarthritis is the most common form of arthritis, more prevalent in elderly, also
termed to be DIET a degenerative disease as it results in structural and
functional failure of synovial joints. People suffering from this disease
usually experience pain and stiffness in the affected joints. In contrast
to other forms of arthritis, it does not affect other body parts like skin,
lungs, eyes or blood vessels but remains confined to the hands, neck,
knees, hips and lower back. This form of arthritis affects each person
differently with severity varying from mild to unbearable pain.
Osteoarthritis Risk Factors :
Age: It is a major risk factor for Osteoarthritis. The biological changes occurring
due to aging can contribute to cartilage thinning, weak muscle strength,
and oxidative damage which may lead to Osteoarthritis.
Gender: Women have higher risks of developing Osteoarthritis than men and
severity too is more. Besides this, during menopause, hormonal
factors can also play an essential role in the development of Osteoarthritis.
Genetics: Children of parents suffering from Osteoarthritis are at greater
risk for developing this types of arthritis than the children whose
parents did not have Osteoarthritis.
Obesity: It is believed to be the most potent risk factor, especially
in case of knee related Osteoarthritis, as 3 to 6 times of total body weight is
transferred across the knee joint during walking.
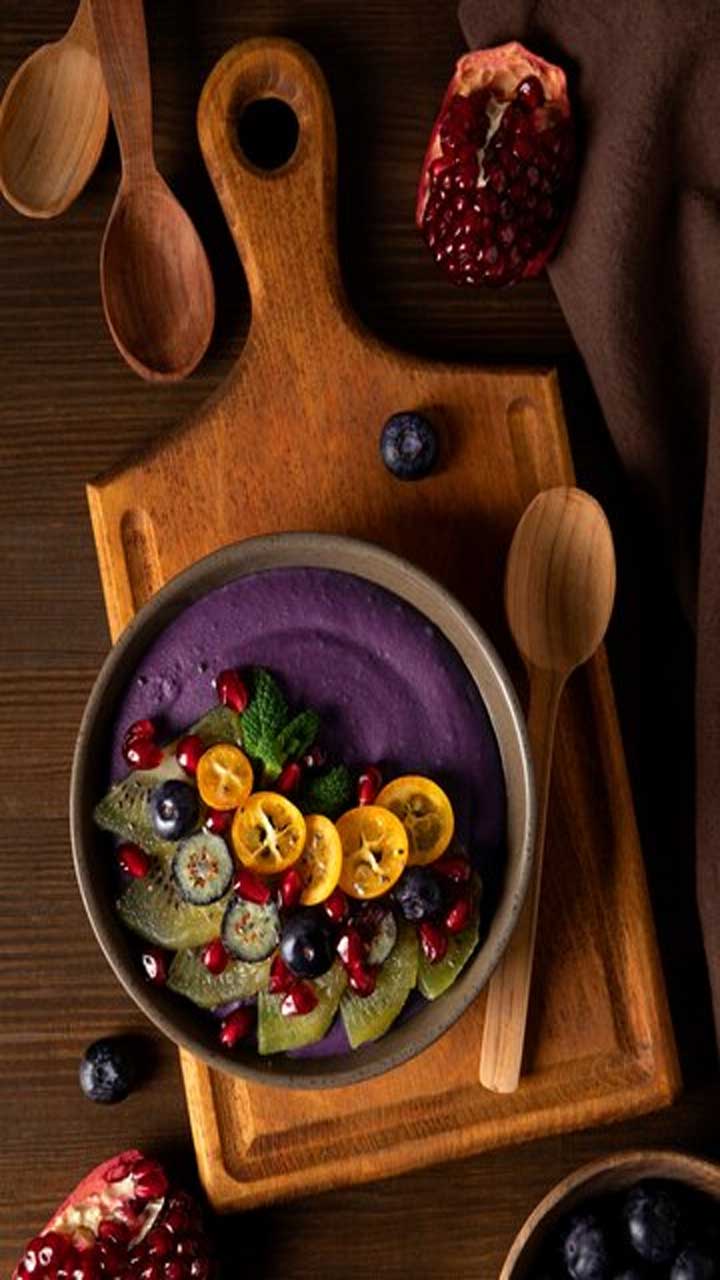
Diet: Individuals with poor diet, with insufficient amounts of
nutrition like vitamin D are more prone to Osteoarthritis, as their bones
can become brittle or thin. Lack of other minerals like selenium,
vitamin C and even vitamin k can cause bone related conditions.
on joints at work is associated with Osteoarthritis. According to studies,
knee related Osteoarthritis risk is more than double in males whose jobs
required heavy weight lifting and squatting than to those who
lacked these physical activities.
Osteoarthritis Affects Body Joints as below
Knee-A Hazard
It is very common, mostly with old age or in obese individuals
with intensity varying from moderate to unbearable. Osteoarthritis can
affect main surface of the knee joint and cartilage under the
knee cap (generally located inside or outside of the knee)
but sometimes also in the shallow depression located at
the back of the knee-joint.
Knee Osteoarthritis is not a localized disease but considered as a
disease of the whole joint resulting from multiple factors
including advanced age, genetics, knee misalignment, low
bone density among others. Several studies have linked
obesity to be the growing risk factor for knee osteoarthritis
due to various reasons. In obese individuals, excess amount
of adipose tissues results in increased synthesis of pro-
inflammatory cytokines which may cause inflammation.
Furthermore increase in weight, increases the pressure
on knees by many folds while doing the daily activities
-Hip-Radiating Pain
Hip joint is one of the largest weightbearing joints in humans
following knees and is likely to be affected by Osteoarthritis. It affects
both men and women equally, and may involve hips. Also
seen to be more prevalent in individuals with hip problems
like abnormal hip development in childhood.
Aging is assumed to cause hip Osteoarthritis mainly due to degenerative
process along with genetics, joint morphology, weight and diet.
Distribution of pain in the body is essential for accurate diagnosis
of this condition. This type of Osteoarthritis leads to pain in the groin, thigh
and knee which is acceptable but, pain radiating down to your
knee (also known as radiating pain) makes its diagnosis difficult.
-Hand- Impairing the Hold
Contrary to the common belief, this type of Osteoarthritis can also occur in
younger individuals, impairing his/her ability to work. Osteoarthritis affecting
hand can negatively impact wrist, fingertips, basilar joint connecting
the thumb and wrist, and middle knuckles of the fingers. Cartilage
present between these joints deteriorates, causing bones to rub
together without a cushion, thereby causing inflammation and pain.
Factors such as age, biomechanical, BMI, genetics and tobacco smoking
contributes as the risks for hand related Osteoarthritis. Moreover, hand injury and
hypertension can also cause this disease. Pain, stiff wrists and fingers
are the certain characteristic symptoms.
-Spinal Column- Affecting the Back Bone
Facets are the only joint found in the spine, therefore, spinal arthritis
means inflammation of the spinal facets. This type of condition generally
occurs due to internal damage causing gradual deterioration of the
cartilage present between the facets. This results in the friction and
further joint injury leading to inflammation.
Stiffness and low back pain (which gets worst in the morning and during
night while sleeping) are commonly experienced by the individuals
Causative Symptoms of Osteoarthritis
-Pain (during movement, may also occur with rest in advanced cases)
-Stiffness
-Reduced function of the joint
-Swelling or deformity
-Joint instability
Tailoring the Physical Test
Tenderness over the joint
Bony enlargement
Restricted joint motion
Altered gait
Muscle atrophy/weakness
Joint effusion
Osteoarthritis Diagnosis and Management
Diagnosis of Osteoarthritis includes clinical examination by the physician,
which is then confirmed by radiography. In advanced stages, Osteoarthritis
is visible in plain radiographs showing bone abnormalities, whereas,
advanced imaging techniques such as MRI or PET-CT Scan can be done to
rule out other possibilities.
The approaches used for management varies according to the condition
of the affected individual. However, aim remains the same which is mainly
controlling the pain, improving the functioning of joint and altering the
disease progress. Management includes:
Non-pharmacological Therapies
Educating the patient about the condition, exercise to increase
the aerobic capacity, weight loss (especially in obese individuals
suffering from knee or hip Osteoarthritis), physical therapies (for joint
movement, muscle strengthening and stretching) and supports
like knee braces or orthotics sums up the non-pharmacological approach.
Pharmacological Therapies
Various analgesics, non-steroidal anti-inflammatory drugs
(NSAIDs), intra-articular corticosteroids and topical treatments
are available to ease the pain.
Surgery
It is avoided till symptoms are manageable by non-pharmacological
approaches or by the use of drugs. Exhausting pain and major limitation
in movement of joints affecting the daily routine generally indicates
surgery. Joint replacement therapy and osteotomy are a few options
which can be adopted in certain severe cases.
What is Rheumatoid Arthritis ?
Joints are an essential part of the body.
When afflicted by any malady they are refrained from performing their
sole function. In Rheumatoid Arthritis, the immune system is unable to distinguish between
self tissues and foreign bodies (like bacteria, virus or fungus). This mistaken
recognition leads to an autoimmune response causing inflammation in
synovial membrane that in turn leads to discomfort in movement of joints,
erosive joint damage and cartilage, and bone destruction.
The onset of disease differs from patient to patient and the severity
depends on the type and pattern of joints involved, as well as the
number of affected joints. High incidence of RA is seen in people
above 50 years of age and females are found to be 3-4 times more
prone to rheumatoid arthritis than males.
Which all Joints gets affected in Rheumatoid Arthritis?
Different type of joint like ball and socket joint, hinge, saddle, plane
and condyloid, function in specific kind of movements and cannot be
replaced by one another. Therefore, a joint once deformed leaves the
person unable to perform certain activities effectively. The joints of
shoulder, elbow, wrist, finger joints, hips, knee, ankle and toe are
commonly affected by Rheumatoid Arthritis. Usually, when Rheumatoid Arthritis proliferates, the first
impact is seen on joints of hands and feet
Coping with Rheumatoid Arthritis
We are blessed to have flexible body which help us move, walk and perform
the daily chores with ease. Our skeletal system possesses junctions, known
as Joints that unites two or more bones and complete the bony frame of our
body. However, these joints can get damaged to a great extent by degenerative
diseases like Rheumatoid Arthritis (RA). Today, this inflammatory condition can
be seen worldwide affecting 1% of the total population across the globe.
How to detect Rheumatoid Arthritis early?
Diagnosis can be done by evaluating medical history, clinical findings,
serological assays (Blood test that looks for antibodies) and imaging
tests. In patients suffering from Rheumatoid Arthritis, identification of the cause of
incipient symptoms may help in better disease management by
retarding Rheumatoid Arthritis spread and degradation of joints. Some tests that
are efficient to evaluate the occurrence of Rheumatoid Arthritis are described below:
Serological and Synovial fluid Analysis
Abnormal ranges of following parameters is the typical feature that
indicate the possible presence of Rheumatoid Arthritis:
- Antibody screening reveals increasing levels of anti-rheumatoid antibodies
and anti-citrullinated protein antibody in serum. It is present in almost 50
to 80% of individuals with RA.
-Erythrocyte Sedimentation Rate (ESR) indicate about the degree of inflammation.
It usually remain elevated in people with Rheumatoid Arthritis.
-C-reactive protein (CRP) is also present in high amount in the sera of Rheumatoid Arthritis affected
individuals. It is found to correlate with the severity and radiographic changes
occurred due to Rheumatoid Arthritis.
Imaging
With the use of imaging techniques, joint inflammation and bone deterioration
can be observed in an early stage of Rheumatoid Arthritis. Some of them are enlisted below:
-Radiography
-Ultrasonography
-Magnetic Resonance Imaging
Estimation of all risk factors and awareness for optimum diagnosis and
treatment gives hope that this disease can be prevented in the near future
Is Obesity Linked to Arthritis?
According to World Health Organization (WHO), obesity across the globe
has more than doubled over the past 30 years.' Obesity has been recognized
since the time of Hippocrates who quoted 'Corpulence is not only a disease
itself, but the harbingers of others which means a medical disorder responsible
for multiple comorbidities.
A common but often underestimated condition- obesity, is defined as excessive
or abnormal fat accumulation in the adipose tissue affecting various organs
directly or indirectly. Generally, this condition develops due to quantitative
imbalance between energy intake and expenditure causing an array of
conditions like type 2 diabetes mellitus, cardiovascular diseases and
coronary heart disease, certain cancers, osteoarthritis, gout and many more.
Obesity and Osteoarthritis (OA)
Osteoarthritis is one of the most common form of arthritis causing a range of disorders
resulting in structural and functional failure of synovial joints. It breaks the
cartilage cushioning of the two joints causing bones to rub against each other
thereby, altering its shape.
The association of obesity and Osteoarthritis was first documented in 1945 by Leach
R.E. and very well stated that 83% of females that suffer from knee
osteoarthritis are obese.' Though, excessive weight causing Osteoarthritis is
widely acknowledged, the exact mechanism causing this is yet
to be fully understood.
Many believe that in obesity, adipose tissue releases extra pro-inflammatory
cytokines (adipokines) which is responsible for inflammation in synovial tissue
leading to Osteoarthritis. Leptin, a hormone, also has a potential link, as its level increases
in obese individuals.
Several non-pharmacological and pharmacological therapies are available
for managing Osteoarthritis. Pillars for non-pharmacological therapy comprise of
exercise to improve strength, avoiding activities causing joint pain,
weight loss and use of aids like cane, brace or crutches to reduce stress
on joint. Among all, weight loss is of utmost importance in overweight
individuals as each pound of lost weight can decrease 3 to 6 folds of
load across the knees. Pharmacotherapy includes intake of oral or
topical drugs and/or intra-articular joint injections.
Obesity and Rheumatoid Arthritis (RA)
The first description of Rheumatoid Arthritis can be found in a dissertation from 1800 by
L. Beauvais which he named Goutte Asthenique Primitive meaning
Primary Asthenic Gout. Persistently, its name has changed several
times till A. Garrod coined the term Rheumatoid Arthritis in 1890.
Rheumatoid Arthritis is a condition which causes inflammation of various joints including
fingers, wrists, shoulders, knees, ankles and other parts resulting in pain,
disability and mortality.
Extra weight increases the amount of adipose tissue which produces
adipocytokines (cytokines secreted by adipose tissue) and inflammatory
cytokines (substance secreted by the cells of immune system which
affects other cells) having immune-modulatory properties impacting
inflammation. Likewise, obesity also leads to vitamin D deficiency and
change in sex hormone levels which can lead to the development of Rheumatoid Arthritis
Several options are available for managing Rheumatoid Arthritis like medications (NSAIDs,
Steroids, DMARDS), therapy and surgery. Surgery is only considered if
medication fails to prevent or slows down the joint damage.
Obesity and Gout
Gout is an old age disease which spans for thousands of years and
appeared in medical records very early. Historically referred as
King's disease' due to its close association with consuming large
amounts of fatty foods and alcohol; as well as obesity.
High serum Uric Acid (UA) levels cause excess deposition of monosodium
urate crystals in tissues, mainly in and around joints like elbow, toe, ankle,
hand and others. Additionally, poor eating habits and lifestyle can lead to
obesity in turn causing high insulin production. Higher levels of insulin
inhibits elimination of uric acid from the kidneys leading to its deposition
at certain joints. This excess accumulation results in gout and gout attacks.
Signs and Symptoms of various types of Arthritis
- Osteoarthritis
Pain, reduced joint functions or movement and joint stiffness can be
experienced along with bony enlargement of the joint, altered gait
and muscle atrophy.
Rheumatoid Arthritis
Fatigue, fever, eye inflammation, anemia, weight loss,
subcutaneous nodules (lump under the skin) or lung infection
Gout
Onset of symptoms occurs suddenly and often during night. Also,
intense joint pain along with joint swelling/redness are observed.
Its management mainly depends upon lowering the blood uric acid
level either by change in diet or intake of serum uric acid lowering drugs.
Can an Infection Cause Arthritis?
Arthritis from microbial infection. Isn't it shocking? But yes, it is true. A more
alarming news is that it does not even spare infants from grabbing into it's claws.
Typically it is a malady of the joints that has become common among the general
population yet, not well understood. It is often misinterpreted as a disease of
the elderly, but can attack people of any age group, race or either gender.
What is Septic Arthritis?
Septic Arthritis (SA) is an inflammatory condition of joints wherein joint fluid
and synovial membrane are infected by disease causing microorganisms which
cause deformity and irreversible degeneration. Studies state that around 4-10
out of 1,00,000 people become victims of Septic Arthritis every year. Individuals suffering
from Septic Arthritis experience joints reddening, warmth and swelling with limited motion,
and fever. The signs indicating the presence of Septic Arthritis may vary from one infectious
agent to another.
Origin of Infectious Agents
Most septic joints are a result of microbial colonization in joints which impair
and restrict joint movements following are some common routes on infection
Through wounds
During joint surgery
human or animal bite nail puncture
injections , catheters
Direct Inoculation of bacteria during surgical replacement or reconstruction
of joints has increasingly became a root cause of bacterial arthritis espesially
in knee and hip operations.
How Infection Works?
Severity of the Septic Arthritis depends on the interaction of immune system and
invading pathogen. At the initial stage, microbe enters the synovial
membrane or cavity and colonizes round the joint. Several self healing
proteins like fibronectin released for tissue repair after surgery aid the
pathogenic colonization and its proliferation. As the disease progresses
an acute inflammatory response is activated by the invading species.
Sometimes these inflammatory responses from the infectious
pathogens may evolve more slowly to become chronic worsening
the patient's condition
Vulnerable Joints
Although infection can occur to any joint of the body, knee and hip
followed by shoulder, wrist, elbow and joints of the fingers are mostly
affected by Septic Arthritis. Few species of Streptococcus and Staphylococcus
are found to primarily affect joints of fingers, wrists, elbow, knee and
ankle. In small children, hip infection is more frequent. Other
joints susceptible to Septic Arthritis are sacroiliac joints (joint between sacrum and iliac),
generally get infected by ingestion of unpasteurized dairy products.
Also, soil exposure (gardening) may lead to the development of disease
in hand and leg joints.
Diagnostic Approaches
Investigation of abnormality related to joints is of utmost importance and
should be diagnosed timely Following diagnostic techniques are considered
viable to confirm Septic Arthritis.
blood testing reveals WBC count, erythrocyte sedimentation rate and
C-reactive protein levels in the blood of Septic Arthritis patient that increases leading
to the inflammatory responses against the microbe.
Synovial fluid analysis is a culturing technique which is performed by
aspirating the fluid sample from patient and culturing it in blood culturing
tubes to check the microbial growth. It gives almost 50% positive results
among people with Septic Arthritis.
Radiographic imaging is a good indicator that can be used before
starting specific Diagnostic Test. It is able to analyze swelling, fluid
ccumulation and narrowing of joints due to cartilage destruction in
later stages of illness or during treatment
Magnetic resonance Imaging (MRI) shows better resolution of soft
tissues near joints and aid in screening of infection in individuals
suspected with Septic Arthritis
Managing Sepsis
To cope up with this painful malady treatment should be undertaken
without any delay thereby avoiding cartilage and joints dysfunction
and disease development. Late detection or recognition of Septic Arthritis leads to
significant increase in rates of morbidity and mortality. Even after
effective management there are chances of relapse or reinfections
Therefore, it is important to aim early treatment, adherence to
prescribed exercises and execute compliance to medication and
therapies in order to keep troubles at bay .
Thyrocare offers rheumatoid factor (RF) Testing, a marker profile for the detection
of rheumatoid arthritis using sophisticated and automated technology at highly
affordable rates.