Obesity has become a worldwide problem whose prevalence is increasing by each passing day. If referred as a
disorder, it is just a century old, in fact, the term obesity appeared in the English language in 17th century with
the description of 'excessive fatness or corpulence'. Yet, its root can be traced back to 20,000 years ago in the
form of mysterious female figures in stone sculptures of Europe. Back then when food was scarce, the humble
beginning of humans as a species, struggling to survive in a place which offered few options between feast and
famine, being obese was considered as the sign of wealth and prosperity. However, health consequences of
obesity began to be noted in 18h century as causes of fatigue, gout and breathing difficulties. Over the past 60
years its exponential increase at an alarming rate led the World Health Organization to declare it as a global epidemic
Obesity is defined as abnormal or excessive fat accumulation in adipose tissue which can impact the overall health.
This fat distribution can be either around the waist and trunk (android/central obesity) or around the body (peripheral
I gynoid obesity). Body mass index (BMI) is a simple and widely used parameter for distinguishing between various
degrees of adiposity. BMI of an individual can be measured by dividing his/her weight in kilograms by the square of
the height in meters (kg/m). BMI over 25 and less than 30 kg/m is considered as overweight or pre-obese, whereas,
30 kg/m or more is considered in the obese range. Generally, obesity can have greater risks of many serious conditions
like type 2 diabetes mellitus, stroke, coronary heart disease, gall bladder disease, osteoarthritis, gout, infertility and
even cancers. Among the several factors responsible for causing obesity, lifestyle and genetics are believed to be the
most common ones.
Lifestyle Factors and Obesity
- Sedentary Lifestyle
Before the modern era, physical requirements were more demanding and required intense physical activity. For instance,
food was gathered by hunting, foraging and later by farming that needed substantial amount of calories. Even making
and maintaining shelters required immense amount of energy. Consequently, modern era doesn't require these physical
activities leading to a sedentary lifestyle and physical inactivity provoking obesity.
Mechanical work associated with muscle contractions during physical activity requires energy. Energy loss due to heat
produced during ATP synthesis and ATP hydrolysis, results in expenditure of energy above the basal level. This affects
the total 24-hour energy use and balance. Additionally, physical activity increases fat free body mass by affecting energy
usage which promotes muscle growth. Fat free mass being the main determinant of resting energy expenditure, its
increase can lead to increased resting metabolic rate which in turn determines the energy balance.
As weight gain results from an imbalance between energy intake and spent, indeed, physical inactivity or sedentary
lifestyle along with the consumption of energy-dense foods can lead to weight gain causing obesity.
- Nutrient Intake
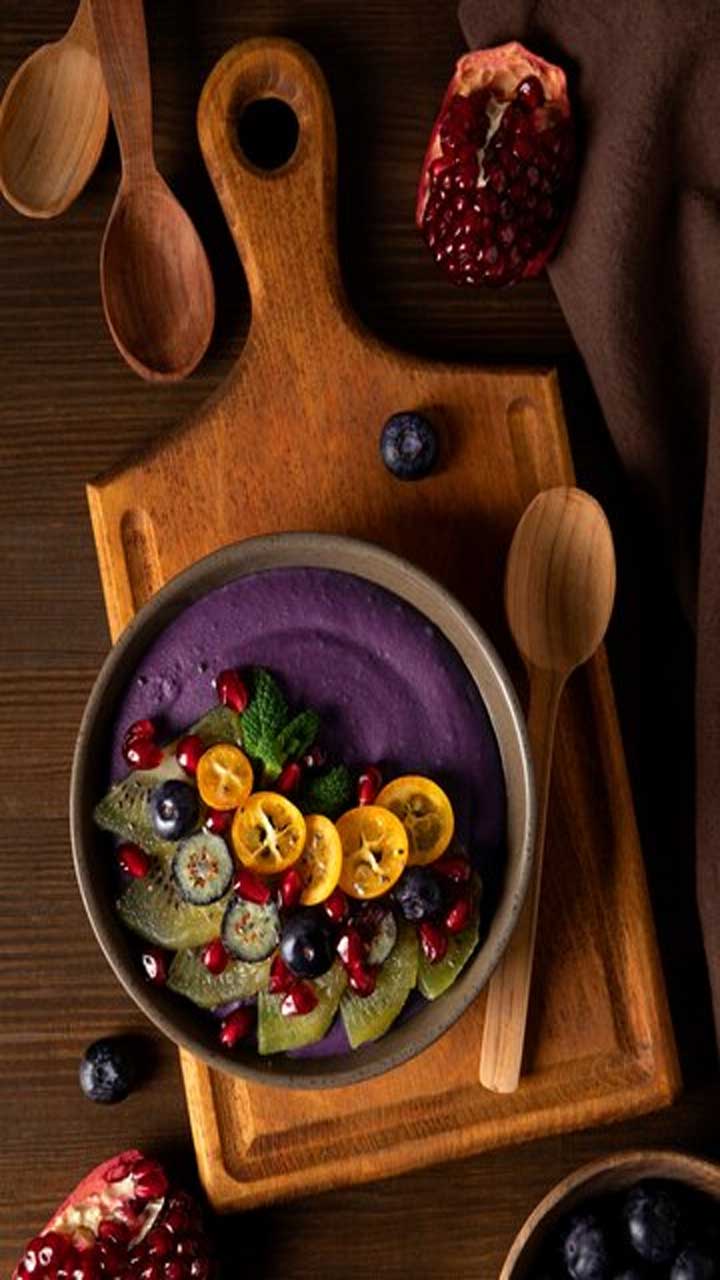
Excessive energy intake through food which are high energy-dense and low nutrient-dense can lead to increased weight,
suggesting long-term negative outcomes. Besides nutrition quality, consuming excessive amount of sugars, salt, alcohol,
saturated trans fat along with limited intake of fibre, fruit, vegetables, grains and certain nutrients also contribute to
obesity. Even, excessive intake of healthy foods can increase postprandial fat deposition. Another risk factor which is
known to increase weight is the consumption of food which are processed.
- Alcohol
Humans are consuming alcohol since prehistoric times for different reasons. Presently, alcohol consumption has
become more common across the globe causing various health and social problems. Although, the impact is less
when consumed in moderation, excessive consumption can damage the liver at a much faster rate and is also linked
with adiposity.
Energy from alcohol acts as an additive to the energy from other food sources. Consuming alcohol before or during
a meal increases the energy density of the meal. Beyond adding energy to the meal, alcohol may also trigger food
intake by amplifying the individual's perception of appetite in response to food stimuli.
Alcohol influences several hormones which are > linked to satiety. It may influence energy intake by inhibiting the
effects of leptin or glucagon peptide-1 (GLP-1). Alcohol also influences hunger by affecting opioid, serotonergic and
GABAergic pathways in the brain. This leads to the increase in appetite. Lastly, alcohol inhibits the fat oxidation
leading to higher body fat eventually.
- Stress
Today, many individuals are affected by stress. This is mainly due to personal conflicts within family and friends,
low socioeconomic status, stressful work environment, poor self-esteem, lack of social support, imbalanced
home/work life and/or others. Results arising from the prolonged stress can contribute to increased weight
and visceral adiposity.
Stress affects the appetite and dietary preferences. Furthermore, men and women who are already overweight
or at the upper limit of normal BMI, are more likely to gain weight due to stress than the one's having lower BMI.
It is due to the fact that, in heavy individuals, elevated insulin levels are observed which is responsible for triggering
weight gain in response to stress. In several cases, it is seen that high cravings for food rich in sugar or fats cause
increase food intake during stress. This effect is thought of as nonhomeostatic feeding which activates brain reward
systems and dampen stress responses. For some obese
individuals, palatable food is thought as an addiction leading to its over consumption. Chronic stress along with the
easy access to palatable and energy-dense foods with no or little physical activity beautifully sets the stage for
development of obesity.
- Sleep
Sleep; a restorative process of the brain is important for overall health of the entire body. Sleep curtailment is
now becoming an endemic with the increase in evening and night-time active hours for work and leisure activities.
Less sleep is linked to obesity by multiple pathways. Alteration in appetite-regulating hormones and upregulation
of the orexin neurons activity can affect the food intake. Likewise, ghrelin, a hunger promoting hormone also
increases along with decrease in leptin (a hormone which contributes to satiety perception) due to the sleep restriction.
Sleep loss also affects the Orexin system which represents the link between sleep and food intake. Homeostatic
feeding center present in the hypothalamic arcuate nucleus is regulated by Orexigenic neurons which affects
hedonic feeding concurrently. Altered levels of leptin and ghrelin hormones directly interact with the arcuate
nucleus, ultimately, modulating the orexin system activity influencing the food intake. Moreover, less sleep could
also sway energy balance by disbalancing the exercise and non exercise energy expenditure.
- Genetics and Obesity
Deoxyribonucleic acid or DNA acts as a code which accounts for the entirety of physiological functions and
differentiation traits among living organisms. It constitutes the molecular framework for evolution allowing
every organisms to adapt in the changing environment. The genetic contribution to obesity has been established
due to the coexistence of several obese members within a family. Despite its high heritability the search for
obesity related genes has been an arduous task. Several approaches have been employed including candidate
gene approach, genome-wide linkage methods and genome wide association studies.
Approaches to identify Human Obesity Genes
- Candidate Gene Approach
It is a hypothesis driven approach which relies on current understanding of biology and pathophysiology of the
disease. The candidacy for a gene is based on: animal models using gene knockout and transgenic approaches;
linkage and positional cloning studies using extreme cases; cellular model systems for their role in metabolic
pathways involved in glucose metabolism. The concept helps in identifying an association between a variant or
mutation within/near the candidate gene and trait of interest like obesity. In order to detect the expected small
effects of genetic variants, this approach needs to be on a large scale and well powered. Till date, several obesity
susceptibility genes have been proposed which includes melanocortin-4 receptor (MC4R) gene, adrenergic B3
receptor (ADRB3) gene, prohormone convertase 1 (PCSK1) gene, brain-derived neurotrophic factor (BDNF) gene
and many more.
- Genome-Wide Linking Studies (GWLS)
It is based on a hypothesis which surveys the whole genome with an aim to identify new unanticipated genetic
variants associated with the trait of interest or a disease. It relies on the relatedness of participants and test,
wherein, certain chromosomal regions cosegregate with a trait or disease across generations. Its survey on whole
genome requires 400-600 highly polymorphic markers, genotyped at 10 pm intervals. Therefore, these studies
have a coarse resolution and identifies broad intervals requiring follow-up of genotyping to locate the genes that
underlie the linkage signal.
- Genome-Wide Association Studies (GWAS)
It is similar to GWLS and interrogates the entire genome, unconstrained by prior assumptions with aims of identifying
previously unsuspected genetic loci associated with the trait of interest or a disease. Thereby, it expands our understanding
and knowledge of the underlying physiology behind that disease or trait by analyzing the whole genome at higher
resolution levels than GWLS. This helps to narrow-down the associated locus with more accuracy and precision. GWAS
can achieve larger sample sizes as it doesn't rely on familial relatedness. With the recent advancements and the production
of smartly designed chips, interrogation of whole genome is now possible in one single experiment.
Obesity-The Genetic Connection
Several studies have shown the coexistence of many obese members within a family. Also, there is around 2-3 fold
increased risk of weight gain among children having obese parents. Along with this, correlation for higher BMI in
monozygotic and dizygotic twins also substantiate the role of genetics in obesity.
In obesity, genetic predisposition has been assumed to affect the energy equation intake/expenditure). However,
Mendelian syndromes having obesity as a clinical feature like Prader-Willi syndrome revealed that reductions in
energy expenditure to be a contributing factor to obesity. Relevant genes are currently being detected via several
approaches like linkage studies including genome wide-scans. These scans even identified specific chromosomal
regions such as those on chromosomes 2, 3, 5, 6 and others. Genes may determine the signals (afferent or efferent)
along with central mechanisms involved in body weight regulation. Already human obesity gene map revealed more
than 425 genes that have direct or indirect link with obesity. Some of these genes are related to dietary intake,
physical activity and energy metabolism among others. Additionally, the genetic linkage between BMI and other
phenotypic characteristics of obesity like fat content, subcutaneous skin fold, etc. are also shown with high
statistical evidences.
So, Is it Lifestyle? Genetics? Or Both!
Involvement of lifestyle and genetics with an individual's weight is well established. Initially, various links were
shown indicating lifestyle factors responsible for obesity. On the other hand, some observations also revealed
that the risk of gaining extra weight was higher in some families than others pointing genetics to be the cause.
In contrast to these facts, the ability of an individual to lose weight, as induced by hypocaloric diets (lifestyle factor)
is influenced by the genotype. Actually, the impact of certain lifestyle factors like activeness or food intake is affected
by the occurrence of mutations or polymorphisms making some individuals more prone to weight gain than others.
Another factor linking lifestyle and genetics to obesity is that all the individuals carrying Trp64Arg polymorphism in
the B3 adrenoceptor gene have an increased risk of becoming obese when they remain sedentary. After all these
factors, yet, future studies are needed to aptly address the interactions of genes and nutrients associated with obesity.